Ureteroscopy FAQs
What is the diagnosis or pathology being treated by this procedure or surgery?
1
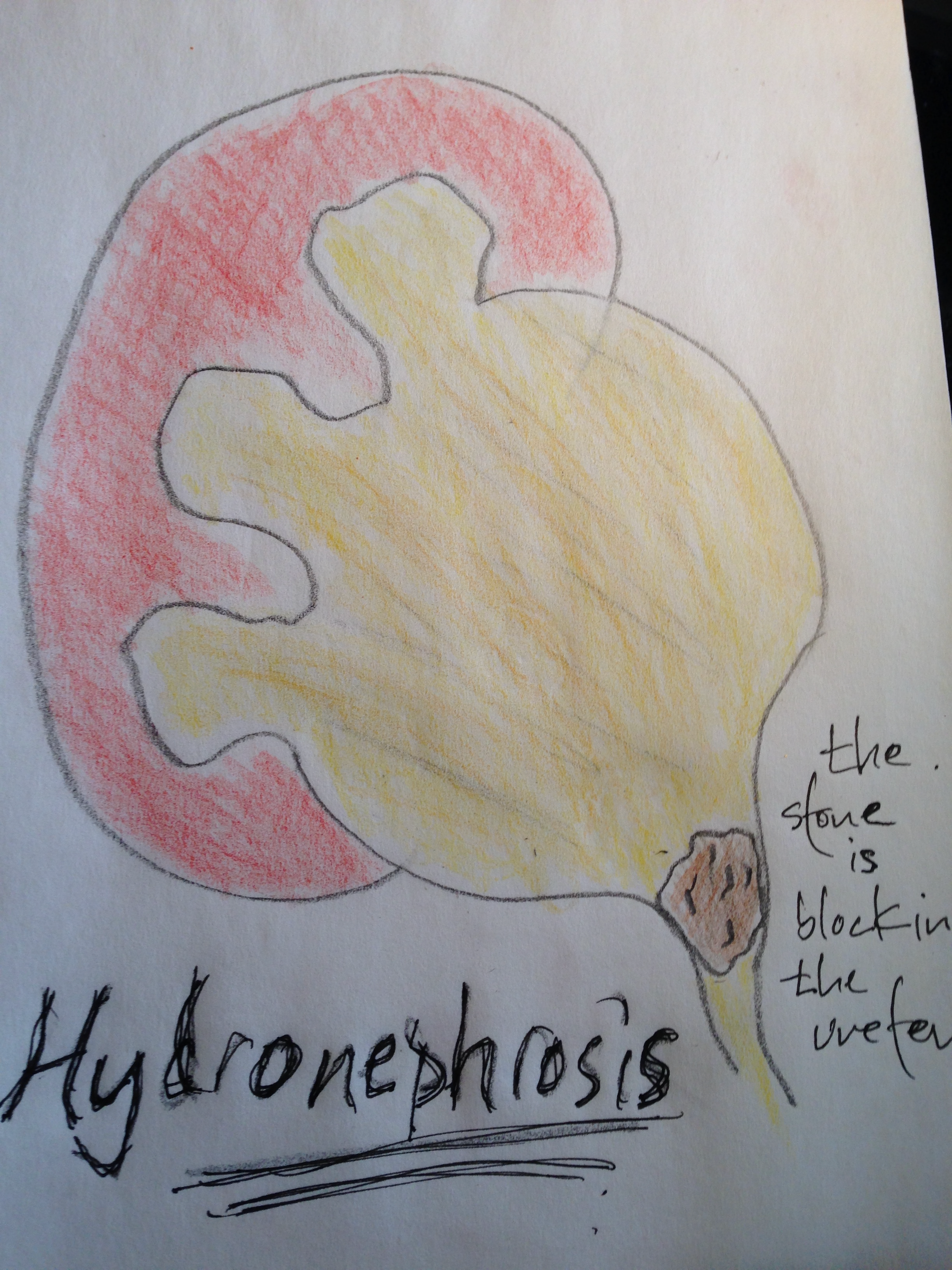
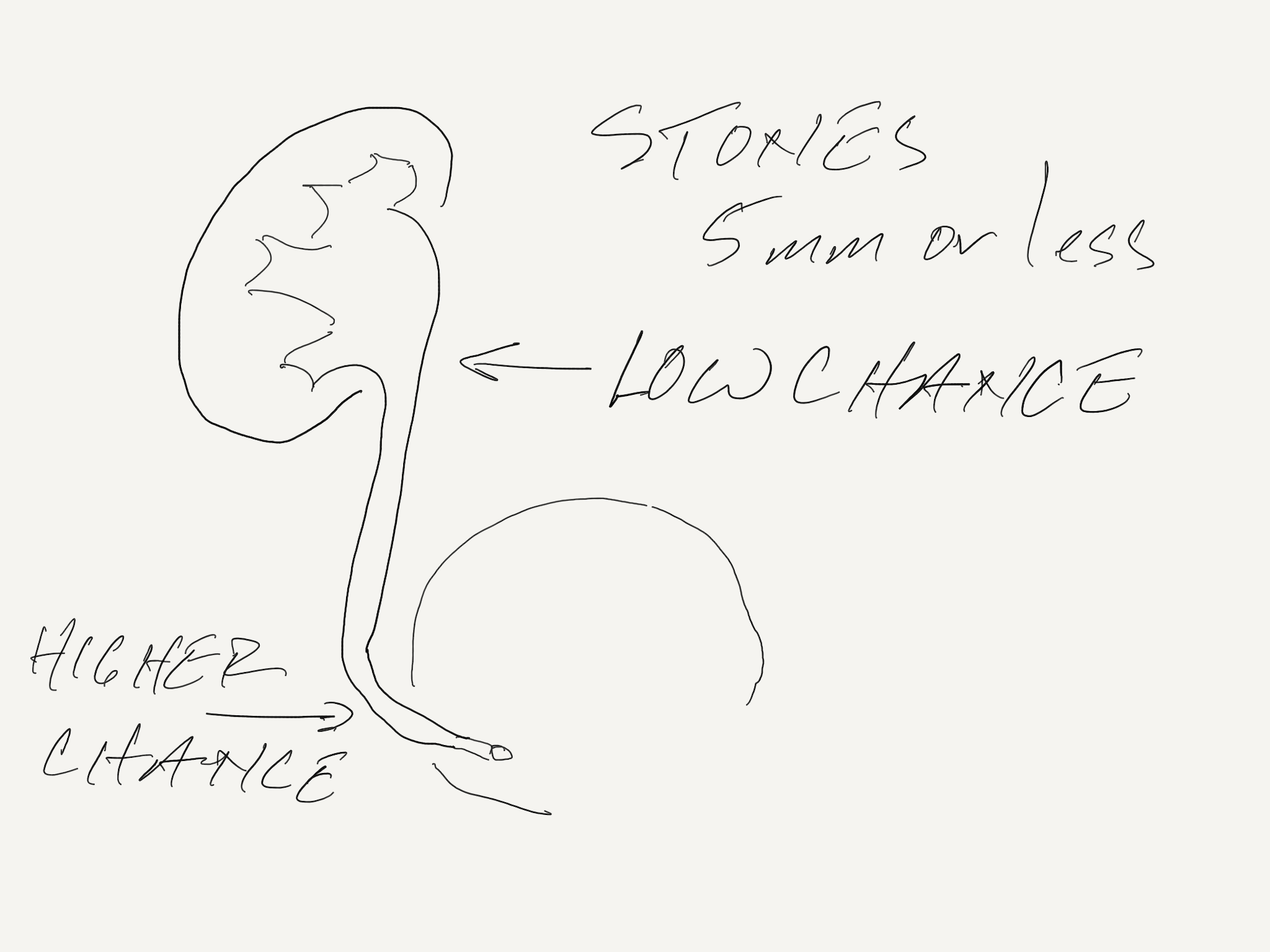
The diagnosis is a ureteral or kidney stone, obstructing or non-obstructing.
Can you describe the procedure or draw a picture?
2
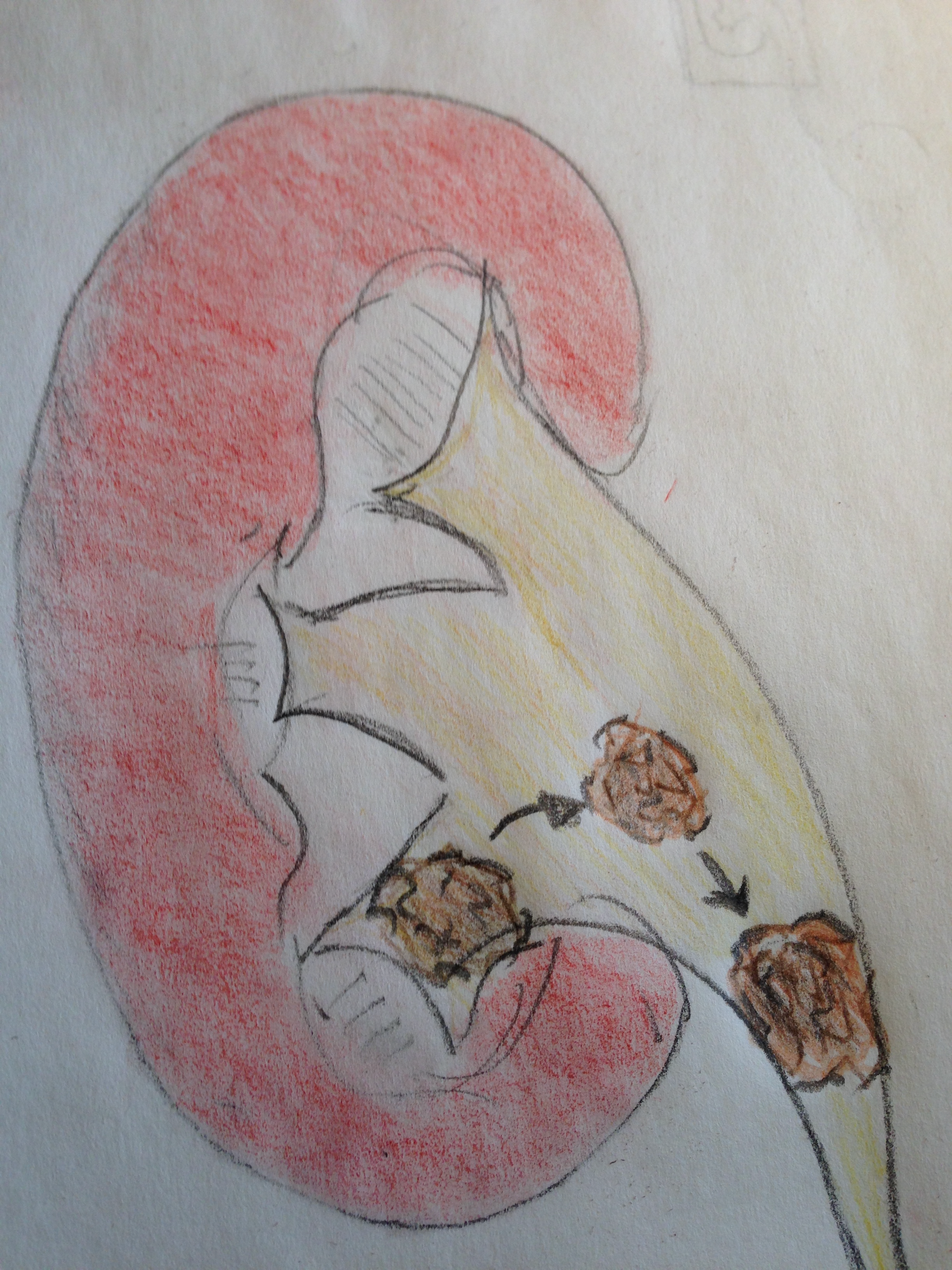
Under general anesthesia a ureteroscope is passed into the ureter to the level of the stone. Small stones may be captured and removed. Larger stones require lithotripsy (fragmentation) most often using a laser.
What are the benefits of doing this procedure?
3
The goal of doing this procedure is to render a patient stone-free.
What are the risks of doing the procedure?
4
Bleeding: Minor bleeding is common and expected. The blood in the urine looks far worse than it is.
Infection: This is a procedure with a high infection risk due to the foreign body (stent) and the obstruction of urine which causes stasis and risk of bacterial growth.
Failure to remove the stone: Stones are hard and the ureter is soft and delicate. There are plenty of times where the stone can’t be removed or be removed entirely with one procedure.
Injury to the ureter: Ureteroscopy should be performed erring always on safety and avoiding injury to the ureter. Ureteral injuries are uncommon.
Anesthetic Risk: The risk of anesthesia is dependent on a patient’s age, health status and clinic condition at the time of the ureteroscopy.
Need for repeat procedure: Because of the nature of the procedure repeat procedures are necessary for some patients. If a stent is placed it dilates the ureter to allow for better access and visualization with a second procedure.
Alternative procedures include Shock Wave Lithotripsy, Percutaneous Nephrolithotomy, or trying to pass the stone spontaneously.
Are there alternatives to this procedure I should be considering?
5
Is this a common procedure?
6
Yes, this procedure is done nearly every day for obstructing kidney stones.
Should I do the procedure now or what happens if I wait to do the procedure?
7
Most obstructing stones need treatment emergently, urgently, or semi-urgently.
How do I prepare for this surgery?
8
Standard precaution exist for most patients including pre-operative evaluation, diet restriction and avoidance of blood thinning medication.
How do I recover from this procedure?
9
The procedure is done outpatient. Most patients will require a ureteral stent. The stent causes bleeding, infection risk, some discomfort. Patients with good pain control can resume normal activity within a few days. The stent will usually be removed 5-10 days after the procedure. For patients who need repeat procedures the stent may remain in place until that procedure is performed.
Is this procedure covered by insurance?
10
Yes, this is covered by insurance.