BPH: Enlarged Prostate
BPH (Benign Prostatic Hyperplasia) is an enlarged prostate. BPH is not cancer. It does not cause or lead to cancer.
BPH is common. After age 40 a man’s prostate begins to grow and change. About half of all men between ages 51 and 60 have signs and symptoms from an enlarged prostate. Up to 90% of men over age 80 prostate-related problems.
As the prostate enlarges it presses against the urethra, restricting the flow of urine. The restriction of flow leads to a slow urinary stream, urinary hesitancy, an interrupted stream,incomplete emptying and getting up at night to urinate. Urine obstruction can also lead to urinary frequency and urgency as the bladder muscles compensates for the obstruction.
If you are a man over 50 with urinary symptoms the most likely cause is BPH. Symptoms include: feeling that the bladder is full, even right after urinating. Feeling that urinating "can't wait". A weak flow of urine. Needing to stop and start urinating several times. Trouble starting to urinate. Needing to push or strain to urinate. “Urgency” of urination. “Frequency” of urination. Getting up to urinate more than 1-2 times a night.
Your doctor can diagnose BPH based on your symptoms and a physical exam in most cases. Sometimes further evaluation is needed such as PSA blood tests, post-void residual urine, ultrasound of the prostate, cystoscopy, urodynamics or UroCuff testing, CT scans or MRI scans
The American Urological Association (AUA) has built a BPH Symptom Score Index. It’s a series of questions about how often you have certain urinary symptoms.
Your doctor will review your Symptom Score and take a medical history. You will also have a physical exam that involves a digital rectal exam (DRE).
The causes of BPH are not well-understood. The male hormone testosterone encourages growth of the prostate (lowering testosterone can cause the prostate to shrink) but there is no explanation why the prostate gets larger under the influence of the testosterone.
There is no sure way to stop BPH. There are medications that can lower the effects of testosterone, but those medications have potential side effects of lowering the testosterone such as sexual dysfunction, metabolic problems of weight gain and heart disease, and loss of bone health.
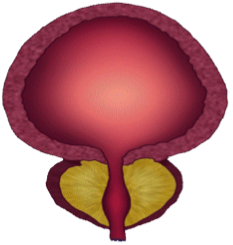
The prostate is part of the male urinary and reproductive system. In a young man it is about the size of a walnut. The prostate is found below the bladder and in front of the rectum. The urethra, which carries urine from the bladder out through the penis is connected to the prostate at the urinary sphincter muscle in the pelvis.
The prostate’s main job is to make fluid for semen and to deliver the fluid during ejaculation.
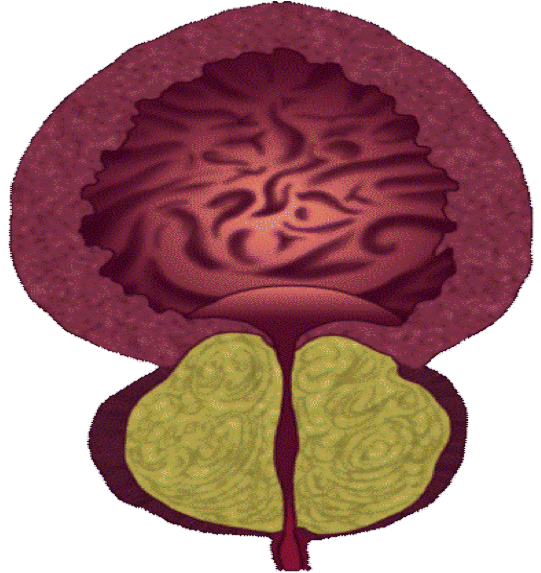
When the prostate enlarges the urethra channel is narrowed by the growing tissue. The narrowing makes urination slower and more difficult to empty the bladder. The bladder responds to the obstruction. The bladder can either stretch to accommodate the poor emptying or, as pictured here, hypertrophy and become stronger to ensure emptying.
Treatment Options
Waiting and Monitoring Your Symptoms
Often, BPH will only require initial evaluation, confirmation of diagnosis, and a watchful approach with no initial treatment. This means that BPH is monitored with regular visits to your physician A yearly exam is common. If your symptoms get worse, or if new symptoms appear, your doctor may suggest that you begin active treatment.
In most men, BPH gets worse with age. Treatment of urinary symptoms lead most men to seek treatment. For mild symptoms men may choose not to treat their symptoms. For men with moderate to severe symptoms treating the BPH can significantly improve quality of life.
For men reluctant to treat their symptoms and who continue to put off treatment, BPH can lead to bladder damage, bladder stones, bladder failure, infection, bleeding, and kidney damage.
Medication Options
For men with moderate to severe symptoms the most common next step is a trial of medication.
“Alpha blockers” relax the muscles of the prostate and bladder. They improve urine flow, reduce blockage of the urethra and reduce BPH symptoms. They do not reduce the size of the prostate. Alpha-blocking drugs include alfuzosin, doxazosin, silodosin, tamsulosin and terazosin. Side effects may include dizziness, lightheadedness, fatigue and trouble ejaculating.
5-alpha reductase (5AR) inhibitors block the production of DHT, a male hormone that can build up in the prostate and may cause prostate growth. These prescription drugs include dutasteride and finasteride. They may take many months to become fully effective.Side effects include erectile dysfunction and reduced libido (sex drive).
The two medications can be taken at the same time, an alpha blocker and a 5-alpha reductase inhibitor used together. Men with larger prostates are good candidates for this treatment.
A urologist may add meidication for patients with overactive bladder symptoms. Overactive bladder is when the bladder muscles squeeze uncontrollably. It leads to the frequent and urgent need to pass urine. It can lead to incontinence (leaking). Antimuscarinics and Beta-3 agonists relax the bladder muscles.
Phytotherapies are herbal treatments or natural supplements. Men buy them over the counter as dietary supplements. One popular option is Saw Palmetto. The herbal therapies do not work as consistently as prescription strength medication. There are many brands available.
Surgery and Office-Based Procedures
Minimally invasive or less invasive surgeries require only tiny cuts or no cuts to the body. Good candidates include men who have taken BPH medication that did not work and the prostate is felt to be an moderately enlarged prostate. They can often be done as an outpatient, without a stay in the hospital. Recovery time is usually quicker. They can offer relief from symptoms, including urine control problems. On the other hand, they do not reduce your risk for another surgery.
Options for minimally invasive treatments include Urolift, ReZum, and Prostatic Artery Embolization.
More invasive treatments require anesthesia and possibly an overnight stay in the hospital. Although these treatments are more invasive initially, they do provide better long term relief of obstruction by removing more tissue.
Example of more invasive procedures include a transurethral resection of prostate (TURP), Laser vaporization (TUEVP), Holmium Laser Enucleation (HoLEP), Aquablation, Robotic “Simple” Prostatectomy.
Choosing the right type of surgery for you depends on the size and anatomy of your prostate, your overall health, and your personal choice.
Let’s first look at the size of a man’s prostate. A “normal” prostate is about the size of a walnut, about an inch and a half in length and width and an inch in height. The normal prostate volume in young men is 10-20 cc. An enlarged prostate begins to cause problems at sizes around 30-40 cc, with more difficult to treat prostate sizes growing to 80cc or more. An extra-large prostate volume can exceed 300cc.
Size matters. The larger prostate requires more tissue to be removed to successfully relieve obstruction. Because procedures vary widely as to how much tissue can be removed, the choice of surgery will depend on prostate size.
The size of a man’s prostate can be estimated by prostate exam but can be estimated much more accurately by prostate ultrasound, MRI, or CT scan.
The shape of a man’s prostate also matters. Prostates do not enlarge uniformly. Most all BPH will grow asymmetrically and lobular. This means that the left and right sides of the prostate will not be the same size. More importantly some prostates have growth at the base of the prostate gland, growing into the bladder lumen as a lobe of tissue that can obstruct the bladder opening. Care must be taken regarding choice of procedure based on prostate shape.
The shape of a man’s prostate, and its growth into the bladder, is best evaluated by a cystoscopy, a scope procedure through the urethra.
Listed below are options that are available as of this writing at the end of 2025.
UROLIFT
The UroLift treatment uses tiny implants to hold open the obstructed prostate. This procedure is often performed in the doctor’s office as an outpatient procedure. This procedure typically is used for men with smaller, symmetric prostates without central lobe growth into the bladder. You can easily find more information at Urolift.com.
ReZUM
Rezūm Therapy uses injections of steam into the enlarged prostate tissue to destroy the BPH and relieve obstruction. The procedure is typically performed in the office as an outpatient procedure.
During each treatment, sterile water vapor is released throughout the targeted prostate tissue. Over time, your body’s natural healing response absorbs the treated tissue, shrinking the prostate. With the extra tissue removed, the urethra opens, reducing BPH symptoms. Unlike other less invasive therapies, this therapy can treat men who have a middle lobe of the prostate.
You can find more information at ReZum.com.
PROSTATE ARTERY EMBOLIZATION (PAE)
PAE is performed by an interventional radiologist as an outpatient procedure. The arteries to the prostate are obstructed reducing blood flow to the prostate and shrinking the gland.
This procedure is best used for men with larger prostate glands who do not want a surgical procedure done under anesthesia in the hospital.
TRANSURETHRAL INCISION OF THE PROSTATE (TUIP)
TUIP is not commonly done but may be used if you have a smaller prostate but still have major blockage of the urethra at the bladder neck. The surgeon uses a laser beam or an electrical current to make small cuts in the bladder neck, where the urethra joins the bladder, and in the prostate.
Men who have a smaller prostate or do not want a more complete prostate resection but need surgery are good candidates for TUIP. The procedure is less likely to interfere with ejaculation than the more substantial TURP.
PHOTOSELECTIVE VAPORIZATION (PVP)
PVP is a very common surgery for BPH. In PVP, the surgeon uses a laser to destroy obstructing prostate tissue. Several types of lasers can be used for this procedure. The Greenlight and Quanta lasers are used most. The laser has the advantage of both removing tissue as well as stopping bleeding by the hemostatic effect of heating the blood vessels.
PVP is done as an outpatient procedure at the hospital or surgery center.
Good candidates for PVP include men with small- to moderate-sized prostates.
TRANSURETHRAL RESECTION OF THE PROSTATE (TURP)
Transurethral resection of the prostate (TURP) is still considered the “gold standard” for surgery for BPH. Under full anesthesia the surgeon uses the electric resection loop to cut away prostate tissue that is blocking the urethra. The resected tissue is flushed and removed from the bladder during the procedure. The resection loop also can cauterize bleeding vessels. The procedure usually requires one night stay in the hospital and a catheter for 3-5 days.
The TURP procedure has quite a reputation because of bleeding risk is higher during and after surgery and there are well known side effects of TURP that may include retrograde ejaculation, erectile dysfunction, urinary tract infections right after surgery and urinary incontinence.
But the TURP continues to be the treatment of choice for many men because it adapts easiest to a wide variety of prostate sizes and shapes. It also has well known long-term success. As I said, it is still considered the gold standard. Symptoms generally improve markedly. The effects of treatment last for many years in most cases.
HOLMIUM LASER ENUCLEATION OF PROSTATE (HoLEP)
In HoLEP, the surgeon removes the enlarged BPH tissue through enucleation, a process of pushing the obstructing tissue back into the bladder and then removing it through a process of morcellation.
Men usually need to spend one night in the hospital after this procedure.
This procedure is used for men with large prostate glands, typically over 80 cc
Men having HoLEP have more post-operative stress urinary incontinence compared to the other surgeries.
TRANSURETHRAL WATER–JET ABLATION (TWJA)
This procedure uses high-pressure water jets to destroy excess prostate tissue. The surgeon first uses ultrasound to precisely map the location of the excess tissue and enters coordinates into a treatment plan for aiming high-pressure water jets directed to that area. Following the destruction of the excess BPH, the surgeon inserts another instrument to seal small blood vessels to reduce the risk of bleeding.
This procedure is performed in the hospital and usually requires one night hospitalization.
DAVINCI ROBOTIC SIMPLE PROSTATECTOMY
For very large prostate the da Vinci robot can be employed to remove the obstructing tissue. Under full anesthesia the robotic instruments and camera are placed laparoscopically, and the central obstructing prostate tissue is dissection from the rest of the prostate, relieving obstruction.
Although this is the most invasive treatment, outcomes are typically very successful because of the complete removal of the obstructing tissue. Risk of incontinence is minimal.
Men who require a robotic simple prostatectomy may also be candidates for a HoLEP procedure.
WHAT HAPPENS AFTER TREATMENTS?
For most men, symptoms of BPH improve after treatment. Infection, bleeding, incontinence, and erectile dysfunction may occur after some treatments. In some cases, scar tissue may form. Most all treatments carry some risk of catheterization following the treatment, including the least invasive treatment performed in the office.
Healing typically takes 4-6 weeks after any of the treatments listed above. Procedures that are done under general anesthesia carry additional post-anesthesia risk.
WHAT ARE THE LONG–TERM SIDE EFFECTS OF TREATMENT?
Side effects vary with the type of treatment you choose. Most side effects are temporary, but there are potential long term issues that can occur after any of these procedures.
Most men will have drastically improved urination after surgery. But some men will have scar tissue after surgery that may cause obstruction and may require additional treatment or surgery to relieve obstruction.
Sexual activity can be affected. If a man can have an erection before BPH surgery, he will probably be able to do so after surgery. That is different than treatment for prostate cancer It may take a while for sexual function to fully return after some procedure. The incidence of erection problems after surgery increases with the more invasive procedures.
Most men will experience a difference in ejaculation after the procedure. Retrograde or absent ejaculation (when semen enters the bladder rather than being sent out through the penis) is the most common ejaculation issue. Men still orgasm during sexual activity, but there is no semen production. The incidence of ejaculation changes increases with increasing invasiveness of procedure.